The most serious clinical problem in this topic, which can affect almost every person living in our climate zone, is the widespread phenomenon of vitamin D deficiency in the winter months. Deficiencies associated with lack of vitamin D are in turn causing other medical problems: abnormal diagnosis of osteoporosis and hyperparathyroidism in people with vitamin deficiency and immune system disorders.
- What is vitamin D and how does it work?
- Why is vitamin D deficiency a common problem?
- Impact of vitamin D deficiency on bone metabolism
- Problem with high concentration of parathyroid hormone
- Other undesirable effects of vitamin D deficiency
- Detection of vitamin D deficiency
- Vitamin D supplementation
- History of vitamin D overdose
- Alternative medicine
What is vitamin D and how does it work?
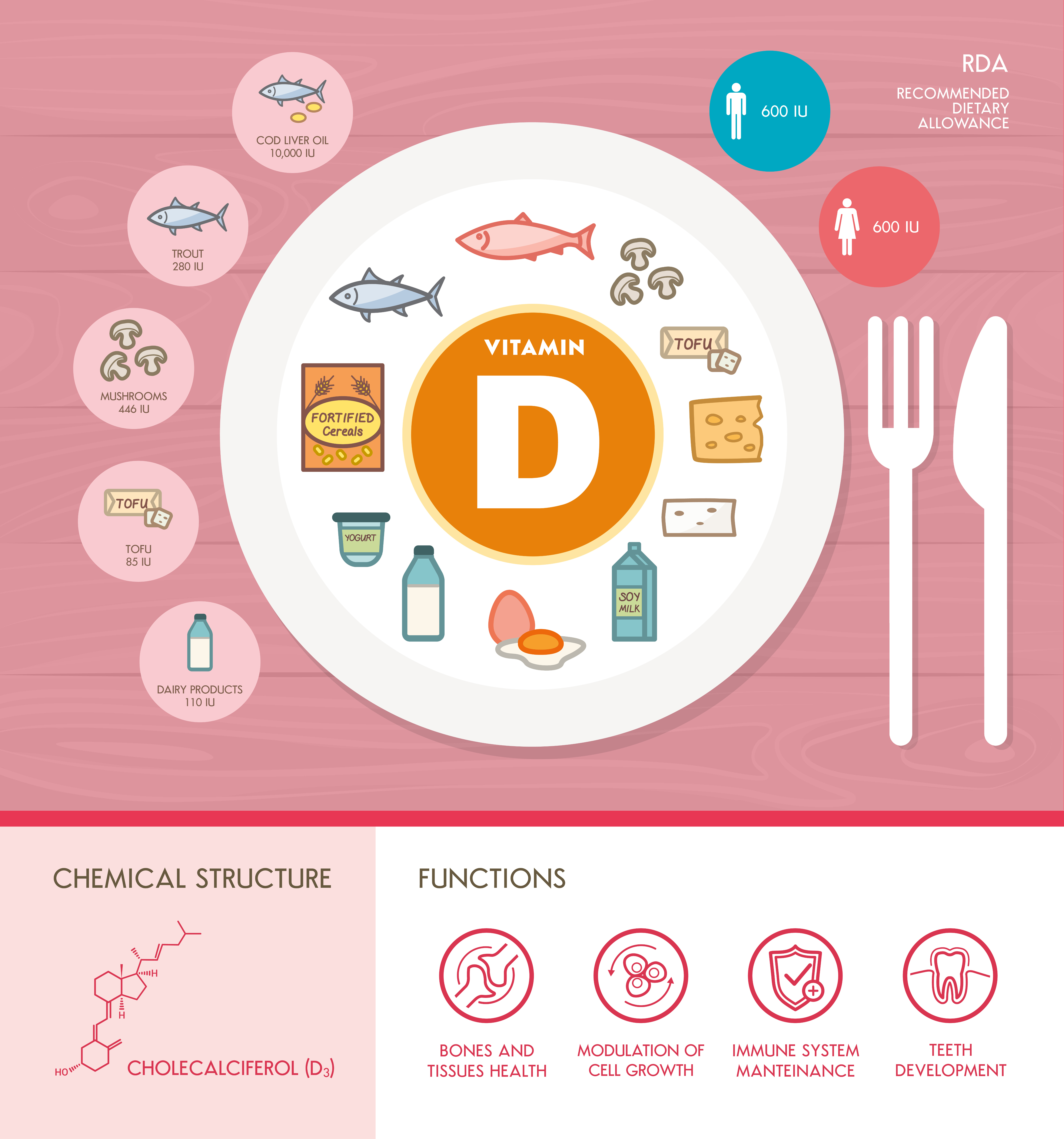
Vitamin D (or more specifically, its D3 version) is a chemical called cholecalciferol - a steroid compound, a cholesterol derivative. It is synthesized in the skin under the influence of ultraviolet. Another version of this vitamin is ergocalciferol (D2) of plant origin. Vitamin D1, which is a component of carbonate, has been found to be a mixture of cholecalciferol and lumisterol, a compound of similar structure but without vitamin D activity. These compounds are activated (hydroxylated) into 25-hydroxy derivatives and then 1.25-hydroxy derivatives. This second transformation takes place under the influence of parathyroid hormone (PTH). Another transformation path is the creation of 24,25-hydroxy derivatives. Transformations D3 and D2 are analogous, D3 derivatives are slightly more biologically active.
The active form of vitamin D3, 1.25-hydroxycholecaleferol (calcitriol), is a hormone substance. It has regulatory functions in many organs and tissues, in particular:
- Increases the absorption of calcium and phosphorus in the digestive tract
- It performs regulatory functions in the immune system (immune)
- It has regulatory functions for its own synthesis - it creates a negative feedback loop and enhances the conversion of D3 into a competitive metabolite of 24,25-hydroxycholecalferferol.
24,25-hydroxycholecaleferol acts anti-absorption - inhibits bone demineralization.
Why is vitamin D deficiency a common problem?
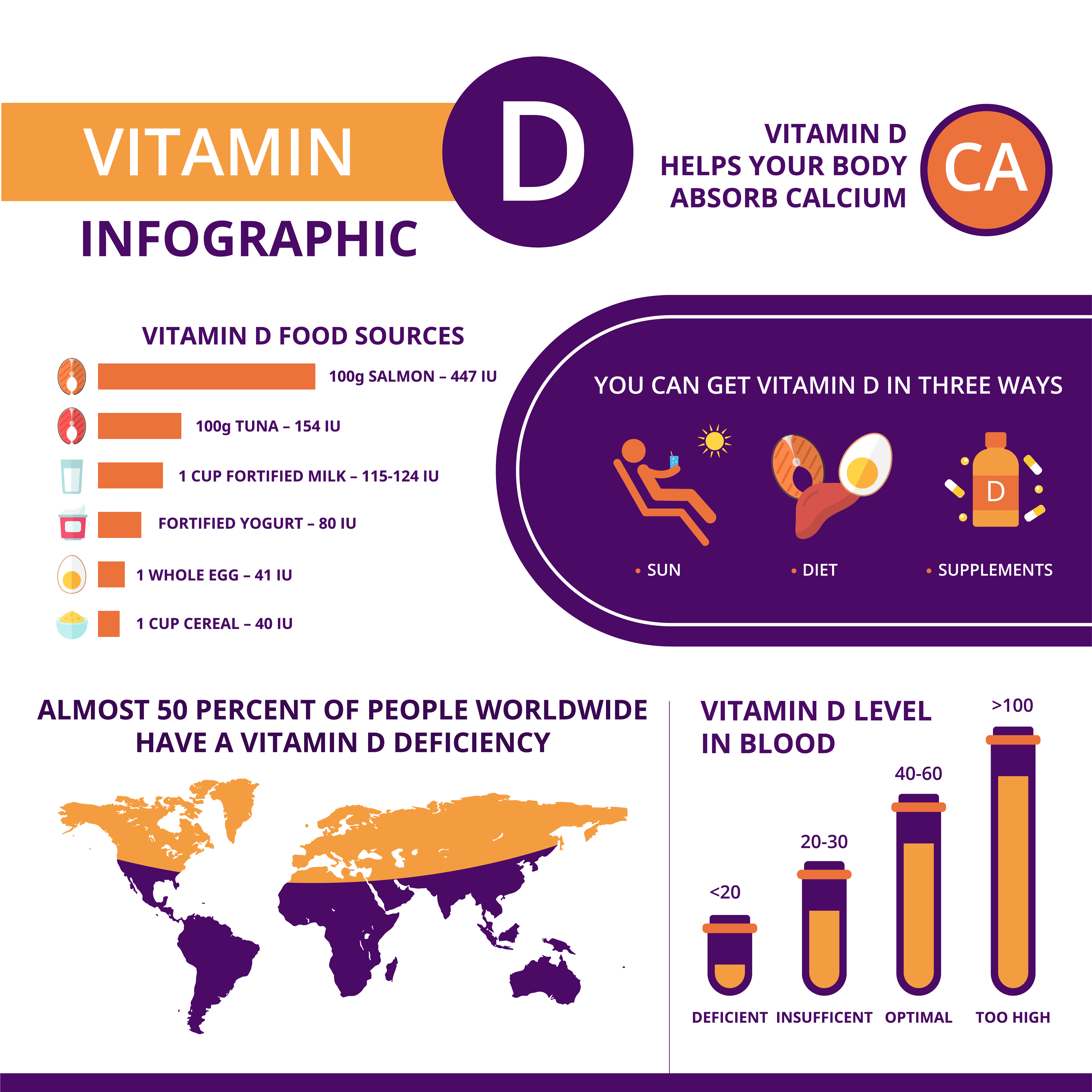
In the latitude in which we live, the angle of incidence of sunlight in the autumn and winter months is too small to produce cholecalciferol in the skin. The amount of "stored" vitamin D3 in tissues is usually insufficient. Epidemiological studies show that the concentration of vitamin D3 or its metabolites in most adults does not reach the desired level.
Impact of vitamin D deficiency on bone metabolism
The correct amount of vitamin D and the undisturbed processes of its metabolism are essential for the absorption of calcium and phosphorus, to ensure the correct amount of these elements in the body. But calcium is not only a bone component, but primarily a component of cellular metabolic processes and signalling systems. In a situation of calcium deficiency, the body devotes bones to choose the "lesser evil":
- Increases secretion of parathyroid hormone (PTH),
- Reduces the synthesis of 24,25-hydroxycholecalcalferol.
As a result, the "release" (demineralisation) of calcium from bones occurs. This results in an increased severity of osteoporosis; in the younger age demineralization of the bone goes without loss of the organic element and is termed osteomalacia. In practice, osteomalacia and osteoporosis are often mistaken for the densitometric detection of abnormal bone mineral density "automatically" is considered osteoporosis.
In children with vitamin D deficiency and associated deficiency of mineralization during the growth period leads to bone distortion, i.e. to rickets.
Problem with high concentration of parathyroid hormone
In practice, I often meet patients who are concerned about elevated parathyroid hormone levels. Usually, the cause of this condition is not primary hyperparathyroidism, but vitamin D deficiency. Its prolonged deficiency can lead to hyperparathyroidism and hyperthyroidism, as discussed in detail in the relevant chapter.
Other undesirable effects of vitamin D deficiency
Calcitriol receptors are found in almost all cells. Its significance has not been fully known. There is no doubt that vitamin D plays a significant role in the immune system, postulated by the association of its deficiencies with:
- Susceptibility to infection,
- Serious autoimmune diseases (immune response to own tissue) such as multiple sclerosis, rheumatoid arthritis or type 1 diabetes,
- Increased incidence of malignancies - especially breast, colorectal, prostate and kidney,
- Carbohydrate-fat disorders - type 2 diabetes and other metabolic disorders accompanying it,
- Increased incidence of cardiovascular diseases such as myocardial infarction and stroke.
This is an incomplete list of the most well-known and previously studied vitamin D deficiency diseases. Vitamin D supplementation is unfortunately not a miracle substitute for all current medical science. There is no full agreement whether Vitamin D deficiency is the cause of all these diseases, or rather their consequence.
People who are sick less often in the sun, take various medicines (which may interfere with the absorption of vitamin D), are often wrecked by illness, so deficiency may be a consequence of the disease and not cause.
Detection of vitamin D deficiency
The concentration of vitamin D3 and its metabolites (25-hydroxy and 1,25-hydroxy) can be determined in serum. The method of determining unchanged vitamin D is considered to be quite unreliable due to its hydrophobicity and its short half-life in serum. The 25-OH-D designation has the advantage that it includes metabolites D2 and D3 and is relatively inexpensive; however, in some disorders of vitamin D metabolism or treatment with certain D3 derivatives may give false information. Lastly, you can mark the active form of D3, calcitriol.
Which sign to choose? This should be consulted with your doctor, as there might be a vitamin D3 activation disorder and it is sometimes worth marking 1.25-OH-D.
Vitamin D supplementation
Should vitamin D3 be taken prophylactically in the form of pharmacological preparations? Yes! When and who should do it?
- 1000 units (IU) from October to April in people avoiding the sun,
- 1000 units (IU) in all people over 65 years old throughout the year, as the ability to produce cholecalciferol in the skin decreases with age.
Such recommendations have been appearing for several years, although the views on this topic are constantly evolving but not quite in one direction - so below are a few comments.
These recommendations concern prophylaxis, a situation where a person without serious health concerns wants to maintain optimum levels of vitamin D3. An example is a healthy adult who had their levels of 25-OH-D3 tested during the summer time and did not detect any deficiency. To maintain this state also in the winter months, the above-mentioned prophylactic doses of vitamin D3 can be used.
It’s a completely different situation when we detect a vitamin D deficiency - such as a child rickety or osteomalacia or other calcium-phosphate disturbance in an adult. A similar case is the diagnosis of severe vitamin D3 deficiency in biochemical studies. Then dosage of vitamin D3 falls within the scope of therapeutic use, much higher doses are under the control of the doctor.
History of vitamin D overdose
The above guidelines for supplementation were adopted on the recommendation of the Britian experts of 2009 (800-1000 IU), the recommendations of the American Institute of Medicine (600-800 IU), and the International Endocrine Society of 2011 (800-2000, obese up to 4000 IU). It’s worth pointing out, however, that the Endocrine Society has set a total daily requirement for vitamin D, so a person on a healthy diet may have a lower recommended dose.
In addition, the Endocrine Society made two recommendations: a dose of 800 IU is necessary for the proper functioning of the skeletal system, a dose of up to 2000 IU may be required if a 25-OH-D concentration of 75 nmol/l (30 ng / ml) The Institute of Medicine found the healthy effect of such a high concentration of 25-OH-D to be unsuccessful, considering it to be a sufficient concentration of 40-50 nmol/l, as 97% of the human population attained intrinsic concentrations of 25-OH-D Up to 50 nmol/l.
The recommendation to take pharmacological supplements at 2000 IU and above was subsequently adopted in a simplified way (without the above, without distinguishing between prophylaxis and treatment) in many recommendations.
There are currently voices criticizing neophyte zeal in vitamin D overdose. In previous studies (the text is updated on a regular basis), unambiguous benefits of supplementation to the extent that 25-hydroxy-D3 concentrations above 40-50 nmol/l have not been confirmed. For example, there are single reports confirming the beneficial effects of high doses of D3 (thereby high concentrations of 25-OH-D3) on insulin resistance and glucose intolerance, but there are also studies on adverse effects, and results can be summarized in other fields of medicine.
It’s advisable to consult a doctor. Broadly cited are experts on the bold thesis on the safety of vitamin D up to 4000 UI and even more. This reasoning is endowed with serious limitations:
- This applies to patients who do not suffer from disorders,
- The safety of such high doses is understood as the absence of toxic symptoms rather than the absence of adverse health effects,
- Fashion for vitamin D causes ill-judged statements of people without enough "read" in the topic.
No one has ever tested the long-term effects of using such large doses of vitamin D for other health indicators. There are currently works suggesting that such radical supplementation in an unmatched population may, however, have negative health effects.
For example, studies on the effect of vitamin D intake on prostate cancer survivability have shown a ”U-curve" dependence, i.e. increased incidence among individuals with both low and high vitamin D intake. Interestingly (and perhaps obviously) it also existed for the intake of other vitamins, especially vitamin C. I would strongly urge our patients to be rational and not discovering the thesis that life is so easy by consuming one vitamin to cure most diseases. If this vitamin has such an important metabolic effect, you must also suffer from the adverse consequences of its excess.
In the British population there is a significant proportion of people with secondary and tertiary hyperparathyroidism (precisely because of long-term deficiency of D3); uncontrolled supplementation causes elevated serum calcium levels and therefore the risk of renal stones, gallstones and pancreatic diseases. The Endocrine Society position clearly states that calcium should be monitored in such individuals. Another common disorder is genetically determined ability of high kidney calcium excretion. The increase in D3 metabolites results in increased "turnover" (absorption and secretion) of calcium in these patients, which may result in kidney stones.
In addition, toxic near-term supplementation is not good at preventing osteoporosis because it results in low parathyroid hormone levels, and this hormone in physiological concentrations has a significant bone-building effect.
Alternative medicine
People with a sense of humour, I encourage you to get acquainted with the alternative iodine treatment - my method, which can replace the use of many supplements and vitamins. It ‘s effective in the treatment or prevention of serious diseases and is most effective in treating the most common disorder of malaise and chronic fatigue.