Probiotics are currently a hot topic, especially for people with irritable bowel syndrome (IBS). IBS is a chronic disease that causes abdominal pain and changes in the intestines. Many people take probiotics in the hope that balancing their intestinal bacteria will reduce nuisance symptoms. This article discusses the latest research on IBS probiotics, including specific bacterial strains and symptoms.
What is IBS?
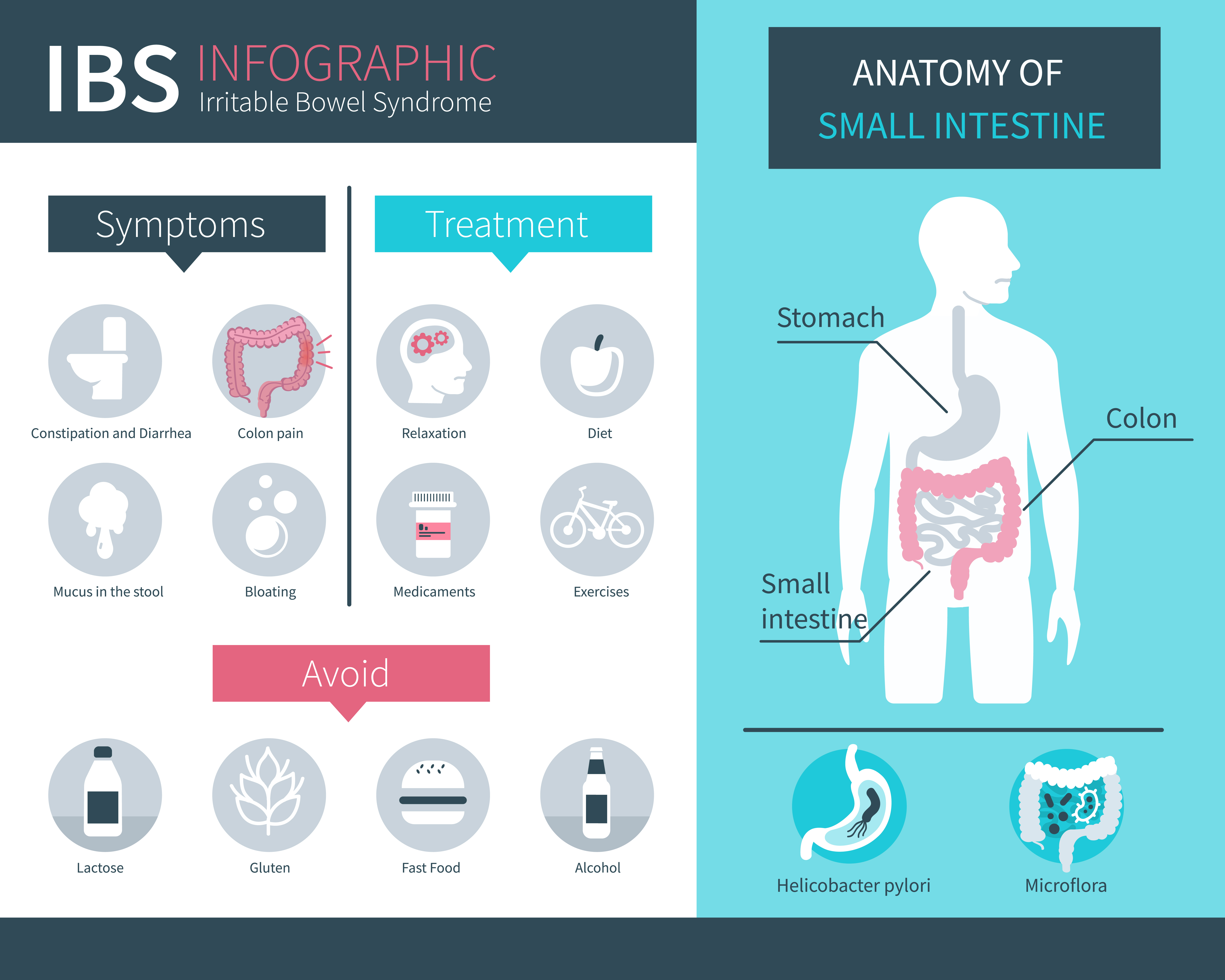
Irritable bowel syndrome is a chronic disease characterized by abdominal pain or discomfort, as well as bloating, gas, constipation and diarrhea (1). It affects 7-21% of people around the world and is three times more common among women than men in the West, although this difference is not so large in Asian countries (1, 2, 3).
The exact causes of IBS remain unknown. However, some of the suggested causes include changes in gastrointestinal motility, infections, brain-intestinal interactions, bacterial overgrowth food sensitivity, carbohydrate absorption disorder, and intestinal inflammation (3, 4). Eating certain foods can cause symptoms, and stress can make them worse (3, 5). An IBS diagnosis is made when you have abdominal pain at least one day a week for three months, and at least two of the following symptoms: pain associated with defecation, change in stool frequency or change in stool appearance (6).
In addition, there are four IBS subtypes that most commonly relate to the type of bowel movement (6):
- IBS-D: Dominant diarrhea
- IBS-C: Dominance of constipation
- IBS-M: Alternately diarrhea and constipation
- IBS-U: Unspecified, for people who do not fit into any of the above categories
Another subtype, known as "contagious" IBS, has also been proposed for people whose disease develops after infections. This subtype can affect up to 25% of people with IBS (3). Treatment of all subtypes includes pharmacological therapy, diet and lifestyle improvement, elimination of FODMAP and lactose, and use of probiotics (3). FODMAP are poorly digested types of carbohydrate molecules found naturally in many foods. They can cause gastrointestinal symptoms, such as gases and bloating, which can exacerbate IBS.
What are probiotics?
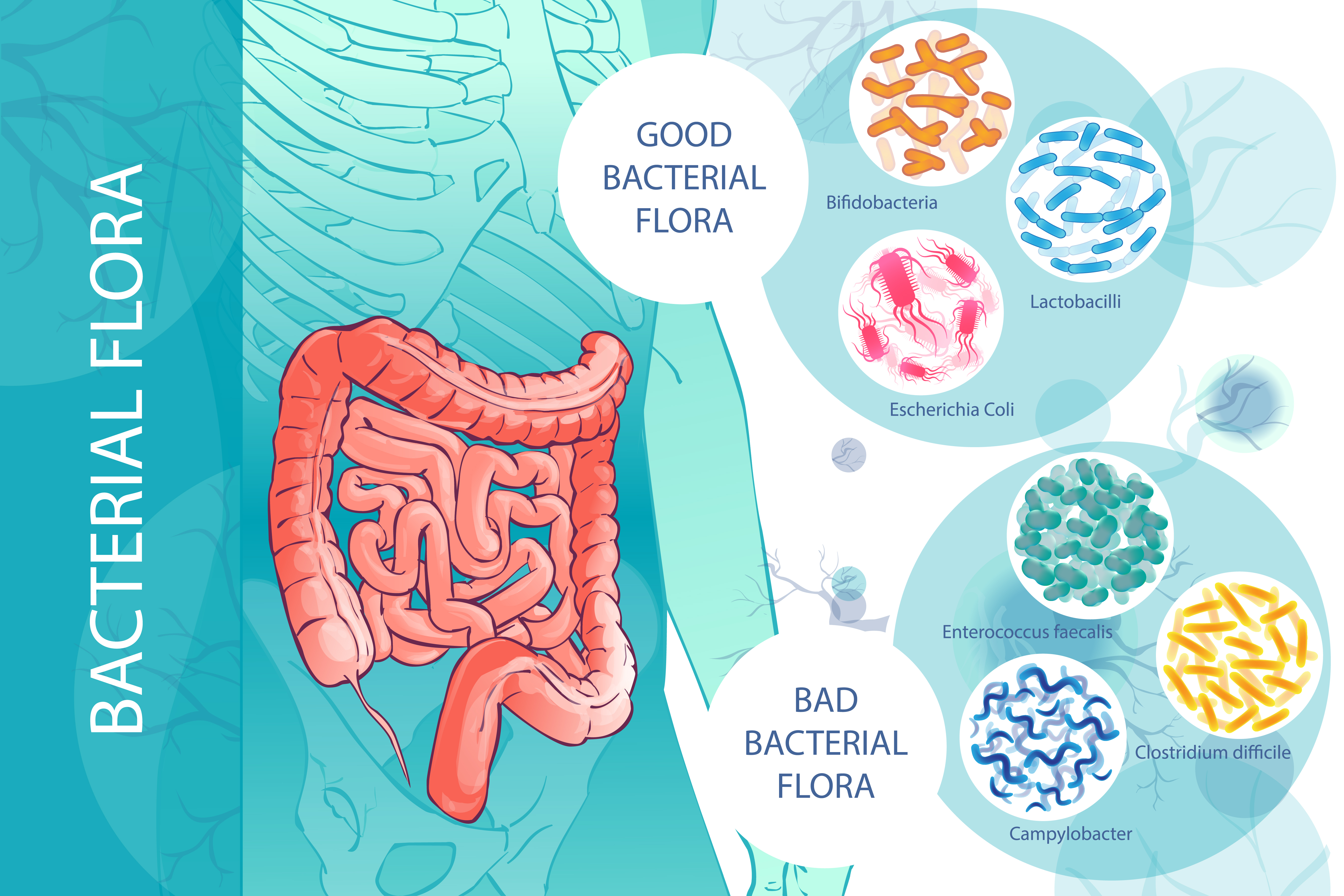
Your digestive system is infested with beneficial bacteria, known as intestinal flora. They play a key role in maintaining the body in good health (7, 8). However, for various reasons, the intestinal flora can sometimes be unbalanced, allowing the reproduction of harmful bacteria (7). Probiotics are live bacteria or yeasts found in food and supplements. They are safe, similar to the natural intestinal flora and provide a mass of health benefits (8).

People use them to maintain a healthy, balanced intestinal flora. They can provide a number of health benefits, such as assisting with weight loss, improving heart health, improving digestion and strengthening the immune system (8, 9). Some popular probiotic products include yogurt, sauerkraut, tempeh, kimchi and other fermented products.
In addition, the popular probiotic strains found in supplements include Lactobacillus and Bifidobacterium (8).
How do probiotics affect IBS?
A significant portion of recent probiotic studies have looked at how they can be used to treat IBS.
The symptoms of IBS are associated with some changes in the intestinal flora. For example, people with IBS have smaller amounts of Lactobacillus and Bifidobacterium in their intestines, and higher levels of harmful Streptococcus, E. coli and Clostridium (7, 9). In addition, as many as 84% of patients with IBS experience bacterial overgrowth in their small intestine, which can lead to many unpleasant symptoms (7).
However, it’s not certain whether this change is the cause or the effect of IBS. In addition, some medicines used to treat IBS symptoms can damage healthy bacteria in the gut (7, 10). Changes in the intestinal flora can affect the symptoms of IBS by increasing inflammation, increasing sensitivity to intestinal gas, reducing immune function and altering the motility of the gastrointestinal tract (7, 11).
Probiotics have been proposed to improve symptoms through (10):
- Inhibiting the growth of pathogenic bacteria
- Improvement of the barrier function of the immune system
- Helping fight inflammation
- Slow bowel movements
- Reducing gas production by balancing the intestinal flora
- Reducing the sensitivity of the intestine to gas accumulation
However, not all probiotics are the same. In fact, the term "probiotic" covers many different strains and types of bacteria and yeasts.
Can probiotics reduce IBS symptoms?
A comprehensive assessment from 2016 showed that it’s not entirely clear how effective the probiotics are in treating IBS. The main objection was the small size of the research and the lack of consistent data (11). However, many studies have shown that certain probiotics can potentially target specific symptoms. Probiotics from the Bifidobacterium, Lactobacillus and Saccharomyces families showed a special effectiveness in action (10, 11).
Reduction of symptoms
A review of 29 studies conducted by the British Dietetic Association (BDA) noted a general improvement in symptoms, and 14 of them showed a positive result for 10 different probiotics (11). For example, 214 IBS patients took part in the study. They took the probiotic L. plantarum 299v. After four weeks, 78% of patients rated the probiotic as good or excellent to reduce symptoms, particularly abdominal pain and bloating (12).
These discoveries were supported by another study in Poland. However, two other, smaller studies of the same probiotic strain did not show a positive effect (13, 14, 15). A German study of the two-component probiotic liquid also had promising results. In this study, 297 patients were treated for eight weeks and experienced a 50% reduction in overall symptoms, including abdominal pain (16).
Meanwhile, Bifido forte is a probiotic containing four strains that has been tested on 186 patients in the UK. A reduction in the overall severity of symptoms after 12 weeks of treatment was found (17). Bifidobacterium breve BR03 has also been shown to minimize pain, bloating and bowel problems in all IBS subtypes (3). While some of these results are promising, there is some inconsistency between the studies. In addition, most strains have only one test showing their effectiveness. Therefore, more research is needed to confirm these extremely promising results.
Abdominal pain
Abdominal pain is one of the main symptoms of IBS. It often occurs in the bottom part of the belly and disappears after defecation (18). Seven types of probiotics were associated with an improvement in abdominal pain (11). It was found that the strain L. plantarum reduces both the frequency and severity of abdominal pain compared to placebo (12).
One of the studies examined the yeast S. cerevisiae, also known as Lesaffre. After eight weeks of treatment, 63% people in the test group and 47% people in the placebo group had a significant reduction in pain. In another study, participants were taking a probiotic solution consisting of B. bifidum, B. lactis, L. acidophilus and L. casei for eight weeks. Their pain decreased by 64% in the group receiving probiotics and 38% in the placebo group. Although the results of these studies are positive, the majority of probiotic studies did not show a beneficial effect on pain.
It’s also interesting to see how the placebo effect had a great impact on these studies. The placebo effect occurs when people experience a positive effect during the study, even when taking a placebo. This is commonly observed in IBS studies (21).
Bloating and gas
Excessive gas production and increased sensitivity can cause uncomfortable flatulence and gases. This is a particularly embarrassing symptom of IBS. In the 2016 BDA survey, only two studies showed that probiotics markedly reduced flatulence, and only one found that they reduced the amount of gas (11). It was found that L. plantarum strain reduces the frequency and severity of bloating symptoms compared to placebo (12).
In another study, patients were given a drink of wild rose berries mixed with oat soup fermented with L. plantarum. The study group experienced a significant reduction in the amount of gas, and both the study group and the placebo group experienced a reduction in abdominal pain (14). An additional study showed that IBS participants experienced reduced abdominal flatulence after four weeks of treatment with a four component supplement containing B. lactis, L. acidophilus, L. bulgaricus and S. thermophilus (23).
Diarrhea
About 15% of people with IBS experience a subtype associated with frequent beats (24). While there are many studies on probiotics in the case of diarrhea associated with infection, less is known about the impact of probiotics on non-infectious types, as in IBS. It has been found that one probiotic known as Bacillus coagulans reduces many symptoms, including diarrhea. However, the current research has been small, so further tests are needed.
The probiotic yeast Saccharomyces boulardii was also examined for the treatment of IBS with the predominance of diarrhea. However, while one study showed improved bowel function and reduced inflammation, others did not show any improvement.
A probiotic with many strains known as VSL # 3 was tested on people with IBS and the intestinal function was slowed down and the amount of gas reduced. However, in the study of people with IBS with the predominance of diarrhea, there was no improvement in stool consistency and frequency of bowel movements. Another probiotic with many strains was tested on 50 patients over eight weeks. There was a significant improvement in stool consistency compared to the placebo group. In general, it seems that the use of probiotics to treat diarrhea in IBS is not very effective because only a few small studies have shown an improvement.
Constipation
The most common form of IBS is the type characterized by constipation affecting almost half of all people with this disease. Studies on IBS with dominance of constipation were aimed at determining whether probiotics can increase the frequency of bowel movements and alleviate the associated symptoms.
In one study, participants were given one of two probiotics with many strains, one of them containing L. acidophilus and L. reuteri, and the other one containing L. plantarum, L. rhamnosus and L. lactis. Treatment with these probiotics caused more frequent bowel movements and improved stool consistency. In a study of children with IBS, treatment with B. lactis probiotic and prebiotic inulin reduced constipation, bloating and a feeling of fullness. However, it should be noted that in some IBS patients, inulin may exacerbate symptoms.
In addition, S. cerevisiae has been found to reduce symptoms of pain and bloating with IBS with constipation dominance. However, further research is needed to confirm this (34). As with most of the other symptoms discussed, while some of these results are promising, previous studies have been relatively small. There has not been enough research to confirm whether probiotics really benefit people with constipation in IBS.
Is it worth reaching for probiotics if you are suffering from IBS?
Despite some promising research, it’s too early to provide general recommendations on the use of probiotics in IBS.
Although it has been shown that some strains benefit from one or two symptoms, most probiotics are unlikely to contribute to a spectacular improvement.
Here are some key tips when making a choice:
- Choose a probiotic that has been appropriately changed
- Choose a probiotic that matches your symptoms
- Take the right dose: Use the dose recommended by the manufacturer
- Do not change probiotics too often: Try one variant for at least four weeks and monitor your symptoms
Probiotics for IBS - summary
Keep in mind that some probiotic supplements contain ingredients that can worsen symptoms. These include oats, inulin, lactose, fructose, sorbitol and xylitol. If your symptoms are caused by any of them, look for a probiotic that does not contain them. Even if you do not experience significant improvement, probiotics still offer other great health benefits and can be a valuable addition to a healthy lifestyle.
Bibliography: