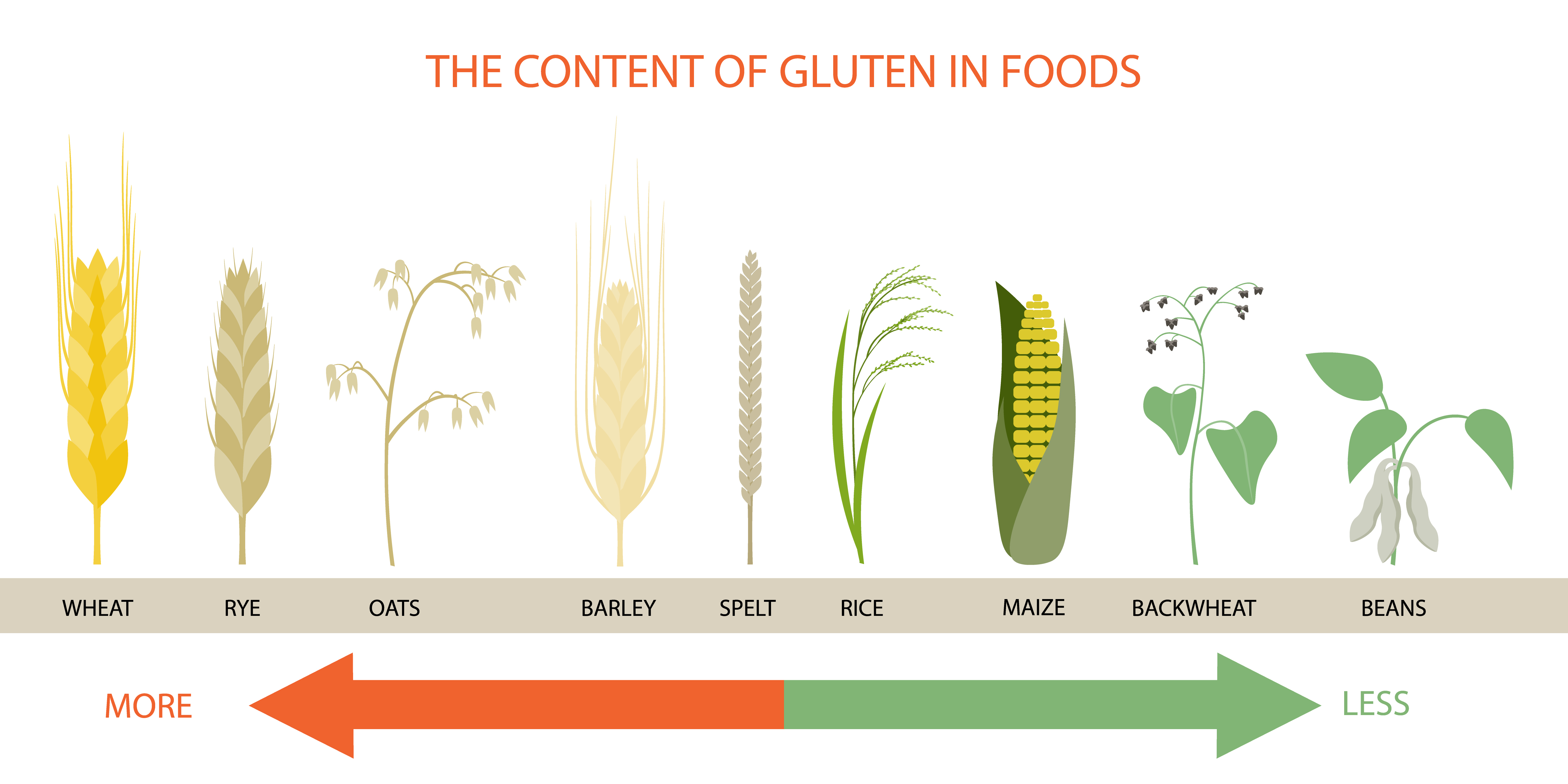
Coeliac disease is an autoimmune condition, caused by a reaction to gluten, a protein found in grains such as barley, wheat and rye. The answer for treatment might seem simple but treating coeliac disease is much more than just steering clear of gluten. Coeliac disease suffers face a number of complicated nutritional challenges.
What's the deal with gluten?
Nutrient malabsorption may have occurred while they were still eating gluten, which could have lead to a number of problems include anaemia, low bone mineral density, osteoporosis or vitamin deficiencies. Also, gluten-free products aren’t usually enriched or fortified with extra vitamins, making it difficult for individuals to obtain enough vitamins, including B vitamins, calcium, vitamin D, iron, zinc, magnesium and fibre.
So what are autoimmune conditions?
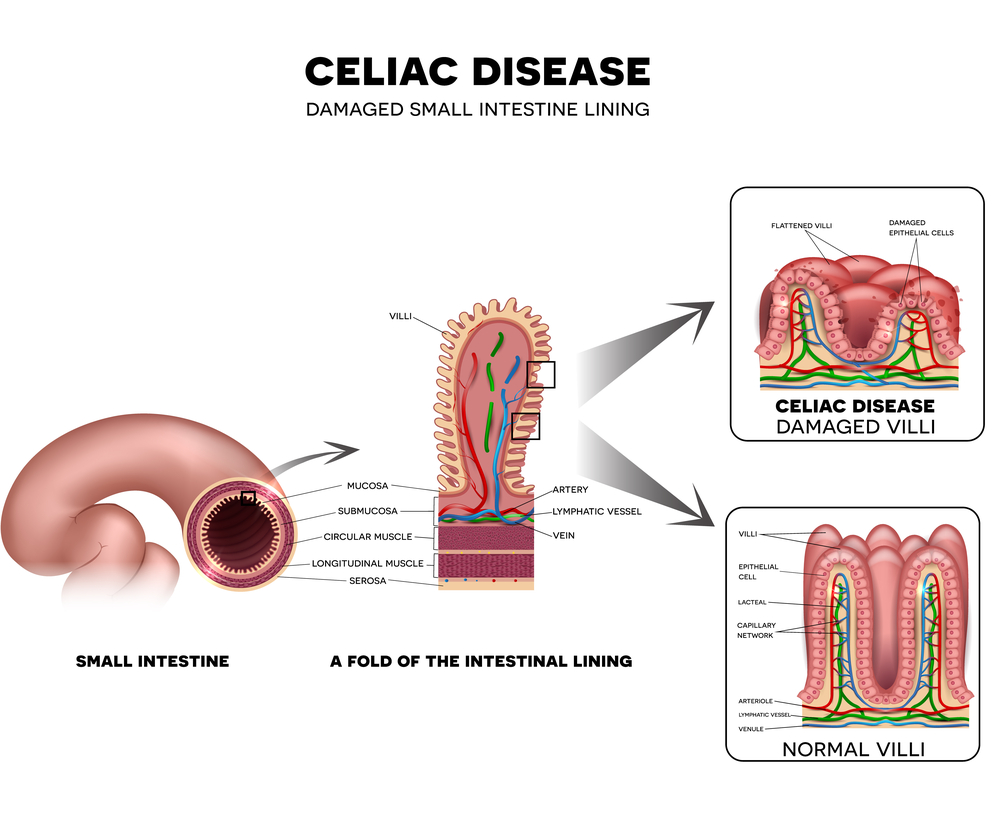
This is where the immune system thinks the body is under threat and mistakes certain healthy cells and substances for harmful ones. The immune system generates a response to this perceived threat and antibodies are released to fight the substance, leading to inflammation. In coeliac disease, the immune system thinks gliadin, a substance that makes up gluten, is a harmful foreign invader and launces an immune attack in response. This reaction causes the intestine to become inflamed and unable to absorb nutrients properly. It can lead to damaged and flattened villi, tiny finger-like projections that line the small intestine. Villi are vital for digestion and absorption of food so it’s not very hard to see why coeliac disease sufferers can easily become malnourished as it’s likely they won’t be absorbing food properly.
What’s the difference between gluten sensitivity and coeliac disease?
While the symptoms of gluten sensitivity can often be very similar to undiagnosed coeliac disease, the two conditions are different. In gluten sensitivity, it is not clear how the immune system might be involved and research suggests that it does not appear to damage the lining of the gut in the way coeliac disease does. There is also some debate around whether gluten is the culprit of gluten sensitivity or if another component in gluten-containing foods is to blame entirely.
What are the symptoms of coeliac disease?
Although varying from person to person, some of the common symptoms include diarrhoea, indigestion, abdominal pain, bloating, constipation, vomiting, tiredness and fatigue, swelling of the extremities and an itchy rash. Some people experience very severe reactions whilst others more mild.
What causes coeliac disease?
The cause for coeliac disease is still unknown. Evidence suggests that the disease can sometimes be triggered after surgery, pregnancy, childbirth, a viral infection or severe emotional stress. There have also shown to be a number of risk factors involved, including:
- Family history
- Previous digestive issues
- Early gluten introduction. Some research indicates that introducing gluten into a baby’s diet before three months old may increase the risk of developing coeliac disease
- Other health conditions. As with most autoimmune conditions, there is an increased risk of developing other conditions including ulcerative colitis, thyroid conditions and type 1 diabetes.
How do I get diagnosed?
The first step is usually a blood test to check for antibodies which, if present, can indicate coeliac disease. However, your test can come up negative even if you have the condition. If your doctor recommends further testing, you are likely to be referred for a biopsy. Including gluten in your diet is important during testing as your doctor needs to see how your body is reacting to it.
If you’re worried about any symptoms you might be having, it’s important to consult your GP.
Treatment
Removing gluten from your diet is the first step for treatment of coeliac disease – to allow your gut to heal and prevent any further damage. If you continue eating gluten then your symptoms could worsen and you can risk serious long-term damage. Gluten-containing foods include pasta, bread, cereals, cakes, pastries, pies, certain sauces, gravies, biscuits etc. Giving up gluten can be a huge challenge but there are lots of resources and support available.
Low bone mineral density often goes hand-in-hand with coeliac disease so ensure that you are getting enough calcium and vitamin D. The British Society of Gastroenterology recommends that coeliac disease suffers should take at least 1000mg/day of calcium.
As previously mentioned, there are other nutrients that need to be kept an eye on too due to malabsorption issues and lack of supplementation in gluten-free products. These include:
- Vitamin B6
- Folate
- Iron
- Vitamin B12
- Thiamin
- Riboflavin
- Niacin
In order to help correct any deficiencies, supplementation may the best route but before you begin any supplement regime, always speak to your GP who may recommend testing for any deficiencies first.